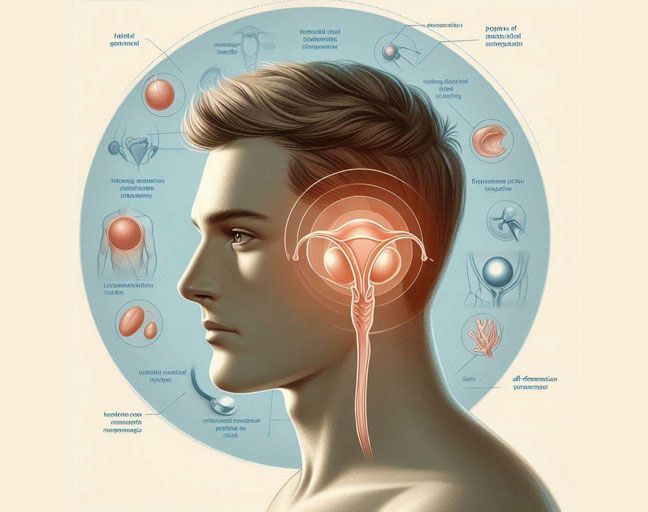
Epididymitis is an inflammation of the epididymis, the tube behind your testicles that carries and stores sperm. When it gets swollen, it can cause pain and discomfort. While this condition can affect men of any age, it’s most common in men between 14 and 35. If you’ve been diagnosed with it, you might be wondering whether it’s an STD (sexually transmitted disease). Let’s clear that up.
Is Epididymitis an STD?
While epididymitis itself is not considered a sexually transmitted disease, the bacteria responsible for causing it are often sexually transmitted. In fact, if you’re sexually active, chlamydia and gonorrhea are the leading culprits behind epididymitis. However, it can also be triggered by non-sexual factors, like infections in young boys or men who aren’t sexually active.
Other causes include:
- Chemical epididymitis: This occurs when urine flows backward into the epididymis, usually from straining or heavy lifting.
- Groin trauma
- Use of urinary catheters
- Tuberculosis: Rarely, this can cause epididymitis.
- Certain medications, such as amiodarone
- Surgical procedures in the groin, prostate, or bladder area
Should I Tell My Partner?
If your epididymitis is caused by an STI like chlamydia or gonorrhea, it’s essential to inform your partner so they can get treated as well. Avoid sexual activity until you’ve fully recovered, as sharing the infection could worsen both your and your partner’s situation.
What Are the Symptoms of Epididymitis?
Epididymitis often presents with a range of symptoms, including:
- Scrotal pain and tenderness
- Swelling around the testicles and groin
- Limping or walking with discomfort
- A burning sensation while urinating
- Redness and warmth around the scrotum
- Fever and chills
- Watery fluid buildup in the scrotum
- Abnormal discharge from the penis (clear, white, or yellow)
The pain usually starts in one testicle but can spread to the entire scrotum or even to the groin area. Although it’s rare, epididymitis can affect both sides of the scrotum (bilateral).
When Should You See a Doctor?
If you’re experiencing pain in your groin or testicle, don’t wait! It could be epididymitis, but it could also be something more serious like testicular torsion. Seek medical help if you’re also having symptoms like burning when urinating, abnormal discharge, or scrotal swelling.
How Is Epididymitis Diagnosed?
To diagnose epididymitis, your doctor will take a detailed medical history, inquire about your sexual activity, and conduct a physical exam. Additional tests might include:
- Urinalysis and urine culture
- Blood tests
- Ultrasound of the testicles
- Radionuclide scanning
How to Treat Epididymitis
Epididymitis isn’t an STD by itself, but if it’s caused by an STI, it will need antibiotics to treat the underlying infection. Your doctor will likely prescribe antibiotics, and it’s essential to take them exactly as directed. The treatment process can take a few weeks, and you may need bed rest, ice packs, and support for your scrotum to relieve discomfort.
If the infection doesn’t clear up after the first round of treatment, your doctor might prescribe additional antibiotics. In rare cases, the infection could last up to three months.
For severe cases, like when an abscess forms, surgery might be necessary. This might involve an epididymectomy, where part or all of the epididymis is surgically removed.
Helpful Remedies
In addition to medical treatment, a few home remedies can help with symptoms:
- Sitz Bath: Fill a tub with about 12 inches of warm water and sit in it for 20-30 minutes to soothe pain and inflammation.
- Herbal Treatments: Three herbs have been known to ease inflammation:
- Pulsatilla: Known for its anti-inflammatory properties, this herb can be used as a tincture or in an infusion.
- Horsetail: This herb has both anti-inflammatory and antimicrobial effects, and can be consumed as a tea.
- Echinacea: Often used in tea, echinacea helps reduce inflammation.
How to Prevent Epididymitis
Although epididymitis isn’t always an STD, practicing safe sex can help reduce the risk. Use condoms and limit the number of sexual partners to protect yourself from STIs.
If you suffer from recurrent urinary tract infections (UTIs), make sure to talk to your doctor about ways to prevent future episodes of epididymitis. Prevention is always better than dealing with the painful symptoms later.