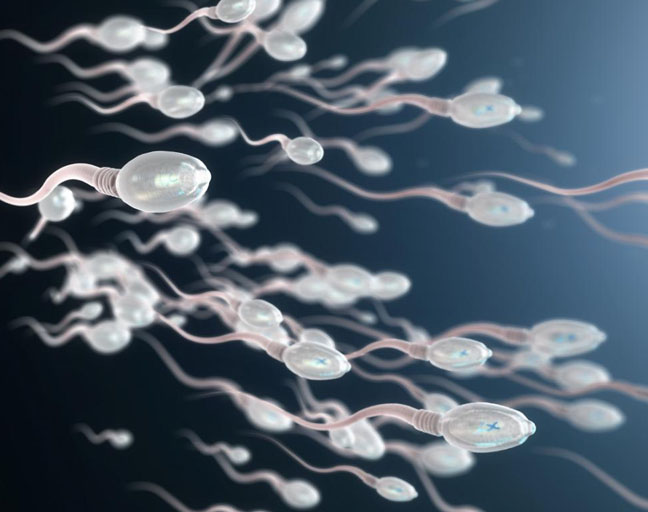
Semen is the whitish fluid containing sperm that’s released by the male during ejaculation. A semen analysis is a medical test that examines the sperm in this fluid, focusing on key factors like the sperm count, shape, and how well they move. Typically, the test involves two or three samples, with results averaged to give an accurate picture of sperm health.
When Is a Semen Analysis Necessary?
A semen analysis is often the go-to test when a couple is struggling with fertility issues. This test helps to figure out if the man’s sperm are healthy enough to conceive and can also point to the possible causes of infertility, such as a low sperm count or poor sperm mobility. It can even help in determining if there’s any dysfunction in the sperm itself.
Additionally, it’s an important part of post-vasectomy checks. If a man has had a vasectomy, the semen analysis confirms whether the procedure worked by showing whether any sperm are still present in the semen sample.
How Should You Prepare for a Semen Analysis?
If you’ve been asked to get a semen analysis, following these simple guidelines will help you get the most accurate results. First, it’s important that the semen sample is between 24 to 72 hours old. This means no ejaculation for 1 to 3 days before your test.
To ensure the test isn’t influenced by outside factors, avoid alcohol, caffeine, and recreational drugs like cocaine or marijuana for about 2 to 5 days before the test. You should also stop taking any herbal supplements, such as St. John’s Wort or Echinacea, beforehand. Be sure to discuss your medical history and any medications you’re on with your doctor. And, if you’re on hormone treatments, it’s best to pause them before the analysis for the most accurate results.
How Is the Semen Analysis Performed?
The first step of the semen analysis procedure is collecting a semen sample. This can usually be done by ejaculation into a clean cup, either at your doctor’s office or, in some cases, at home. Your doctor will then analyze the sample to assess sperm health.
Collecting the Sample
There are a few ways to collect a semen sample, and it’s important to choose a method that works best for you. The most common method is by masturbation, where the semen is directed into a clean cup. Be sure to avoid using any lubricants, as they could contaminate the sample or even kill the sperm.
Alternatively, some men may use a method called “withdrawal” during sex, where the man pulls out just before ejaculation, collecting the semen in a cup. This method is typically used when testing after a vasectomy to ensure no sperm is present, but it’s not recommended for infertility testing.
Another option is using a condom (make sure it’s free from spermicide and other additives). Some clinics even provide these special condoms to avoid contaminating the sample. After ejaculation, seal the condom and place it in the collection cup.
The Process
Typically, you will need to provide two or three separate semen samples within a three-month period to get a good sense of your sperm health. If you’re testing after a vasectomy, it’s usually done 6 weeks after the procedure to ensure no sperm remain.
Precautions for Home Collection
If you’re collecting the sample at home, make sure to get it to the clinic within an hour of ejaculation. Keep it at room temperature—don’t refrigerate or expose it to sunlight, as extreme temperatures can affect the accuracy of the results.
What Do the Results of a Semen Analysis Tell You?
The semen analysis reveals crucial details about the quantity and quality of sperm. The results usually come back within a day, and normal ranges can vary between labs.
- Semen Volume: A healthy sample should have between 2 to 5 milliliters of semen. Anything more or less could indicate a problem.
- Liquefaction: A normal sample liquefies within 20-30 minutes after ejaculation. If it takes longer, it may point to an infection.
- Sperm Count: The sperm count in a typical sample ranges from 20 to 100 million sperm per milliliter. After a vasectomy, there should be no sperm at all.
- White Blood Cells/Bacteria: A normal sample is free from white blood cells or bacteria. Their presence may signal an infection.
- pH Levels: Healthy semen has a pH between 7.1 and 8. Abnormal pH levels can impact sperm motility and function.
- Sperm Shape: At least 30% of sperm should be of normal shape. Abnormal sperm might have multiple heads, tails, or no tail at all, making it difficult for them to fertilize an egg.
- Sperm Motility: At least 50% of sperm should show forward movement within an hour of ejaculation. If they can’t swim toward the egg, conceiving might be a challenge.
Understanding these results helps doctors pinpoint any issues and determine next steps, whether that’s further tests or treatments to improve fertility.