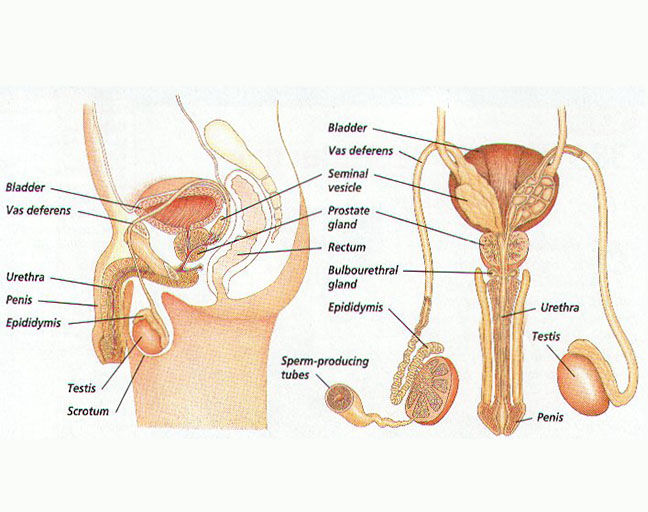
The male reproductive system is a fascinating, intricate setup that plays a crucial role in producing hormones and ensuring reproduction. Its primary job? Making male sex hormones like testosterone, creating sperm, and delivering it effectively. From the external organs you can see to the hidden internal structures, every part works together seamlessly. Let’s break it all down, step by step.
The External Organs of the Male Reproductive System
When you look at the front view of the male reproductive system, the external organs take center stage. These include the penis and the scrotum. Let’s dive into what they do.
1. The Penis
The penis isn’t just a key part of the male anatomy; it’s a multi-functional marvel. It’s made up of three main parts:
- The Root: This is the anchor that attaches the penis to the abdominal wall.
- The Shaft (Body): Cylindrical and elastic, the shaft contains three spongy chambers. These chambers fill with blood during arousal, causing the penis to become rigid—perfect for penetration. Think of it like a balloon filling with air.
- The Glans: The cone-shaped head of the penis, covered by a thin layer of skin called the foreskin. At the tip, there’s the urethral opening—the gateway for both urine and semen.
2. The Scrotum
Just below the penis, you’ll find the scrotum, a pouch of loose skin packed with nerves and blood vessels. Inside this pouch are the testicles, kept at a slightly cooler temperature—an essential condition for sperm production. Imagine it as nature’s version of climate control for fertility.
The Internal Organs of the Male Reproductive System
While the external organs might get most of the attention, the internal structures are the unsung heroes. These include the testicles, epididymis, vas deferens, urethra, and several glands. Here’s how they work together:
1. Testicles
Nestled inside the scrotum, these oval-shaped organs are testosterone factories and sperm-making machines. The seminiferous tubules—tiny coiled tubes—are where sperm cells are born. Fun fact: Most men have two testicles, doubling the efficiency.
2. Epididymis
Sitting right on top of each testicle, the epididymis is like a sperm boot camp. It stores, transports, and matures sperm, preparing them for their big mission. During arousal, contractions push sperm into the vas deferens.
3. Vas Deferens
This muscular tube acts as a highway, transporting mature sperm from the epididymis to the pelvic cavity, just behind the bladder. It’s like a conveyor belt ensuring sperm get where they need to go before ejaculation.
4. Urethra
The urethra’s dual-purpose design is impressive. It’s responsible for expelling urine and, during sexual activity, ejaculating semen. Fun fact: When the penis is erect, the pathway for urine is blocked to ensure semen has the spotlight.
5. Seminal Vesicles
These small pouches attached to the vas deferens produce a fructose-rich fluid—basically an energy drink for sperm. This fluid forms a significant part of the semen’s volume.
6. Prostate Gland
About the size of a walnut, the prostate is positioned below the bladder. It produces a nourishing fluid that mixes with sperm. The urethra runs right through it, making it a vital player in the reproductive process.
7. Bulbourethral Glands
These pea-sized glands, located near the urethra, produce a lubricating fluid. This fluid neutralizes any acidity in the urethra, paving the way for sperm’s smooth journey.
How Does It All Work?
So, how does this complex system function? It all starts with puberty. When a boy reaches puberty, the hypothalamus triggers the release of GnRH (gonadotropin-releasing hormone). This kickstarts the production of key hormones—FSH (follicle-stimulating hormone) and LH (luteinizing hormone)—by the pituitary gland. LH signals the testicles to ramp up testosterone production, setting the stage for sperm creation.
Sperm development takes about 65 to 75 days, with the seminiferous tubules in the testes handling the production. Each day, around 300 million sperm are produced. The epididymis stores and matures them until they’re ready to be transported via the vas deferens. Accessory glands contribute essential fluids during ejaculation, combining with sperm to form semen. Finally, during arousal, the penis becomes erect as blood fills its chambers, leading to ejaculation—the release of semen through the urethra.
Understanding the male reproductive system gives you a deeper appreciation for how every part—big or small—plays a vital role. From hormone production to the journey of a single sperm, it’s an incredible example of biology’s precision and brilliance