The male orgasm is a complex process that involves multiple organs, nerves, hormones, and blood vessels working together in sync. When a man reaches climax, powerful muscle contractions occur (one every 0.8 seconds), and intense pleasure is often experienced. But have you ever wondered, “What does sperm actually smell like?” Here’s everything you need to know about the scent, look, and lifespan of sperm.
What’s the Normal Smell of Sperm?
Typically, sperm has a chlorine-like odor, often compared to bleach. This smell is caused by ammonia and other sterile-smelling alkaloids present in semen. You might notice this scent in places like hospitals, swimming pools, or laundry rooms. Interestingly, about 1 in 5 people can’t detect this smell at all, so some individuals might not even realize that sperm has any odor.
What Affects the Smell of Sperm?
While the smell of sperm can vary, there are a few factors that might influence it:
- Diet: Eating sweet fruits can change the scent of sperm, making it smell slightly different.
- Overall Health and Medications: Your general health and any medications you’re taking can impact how your sperm smells.
- Time: If it’s been a while since your last ejaculation, your sperm may have a stronger scent.
- Smoking and Alcohol: Both of these can give sperm a more bitter odor.
- Sperm Quantity and Quality: The more sperm present, the stronger the scent might be.
What’s an Abnormal Smell?
If sperm develops a fishy or foul odor, or if the color turns brown, red, green, or yellow, it’s a sign of infection. This often happens in the prostate gland or other parts of the male reproductive system. If you notice any of these changes, it’s time to consult a doctor for testing and treatment.
Does the Smell of Sperm Change Over Time?
Interestingly, sperm doesn’t always smell the same. As it goes through different stages, the scent evolves:
- Fresh Ejaculation: Fresh sperm might not smell much at all, or it could have a very light odor.
- Drying Process: As sperm and semen begin to dry, that familiar chlorine-like smell becomes more noticeable, sometimes accompanied by a nutty scent, similar to rancid walnuts or almonds. When fully dried, it can form a crusty, white film.
- Dead Sperm: If sperm is kept in a sealed environment without drying out, it will emit a pungent, unpleasant odor, often likened to that of a decaying corpse.
What Does Sperm and Semen Look and Taste Like?
Curious about what sperm looks like? Here are some details:
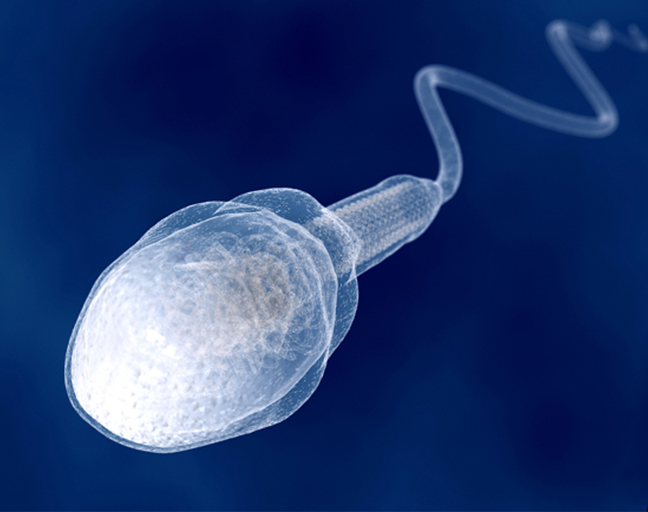
- Appearance: Sperm cells are made up of a head, midpiece, and tail. Sperm, when combined with semen, is usually cloudy white or grayish in color.
- Consistency: Immediately after ejaculation, semen has a jelly-like consistency, but within about 30 minutes, it becomes runnier and clearer. This change helps sperm travel more easily to meet an egg.
- Taste: The taste of semen can vary depending on diet, but it is typically slightly sweet because of the high fructose content.
How Long Can Sperm Live?
If you’re wondering, “How long does sperm live?” here’s what you should know:
- Inside a Woman’s Body: Sperm can live from a few hours to about a week inside a woman’s reproductive system. However, only a small number of sperm survive long enough to fertilize an egg.
- Vaginal Conditions: If sperm doesn’t make it past the cervix, it will only last a few hours due to the acidic environment. But if it does get through, it can survive up to four days.
- Cervical Mucus: During ovulation, when cervical mucus is present, sperm can live up to a week, since the conditions become more favorable for sperm to travel and survive.
- Outside the Body: Sperm typically only survives for about 20 to 60 minutes outside the body, depending on environmental factors. Once the semen dries, the sperm become inactive.
For those concerned about contraception, remember that sperm can also be present in pre-ejaculatory fluid. The withdrawal method is not a reliable form of birth control, so precautions are essential.
Now you’ve got all the answers about sperm’s smell, look, taste, and lifespan, helping you understand the science behind it better!