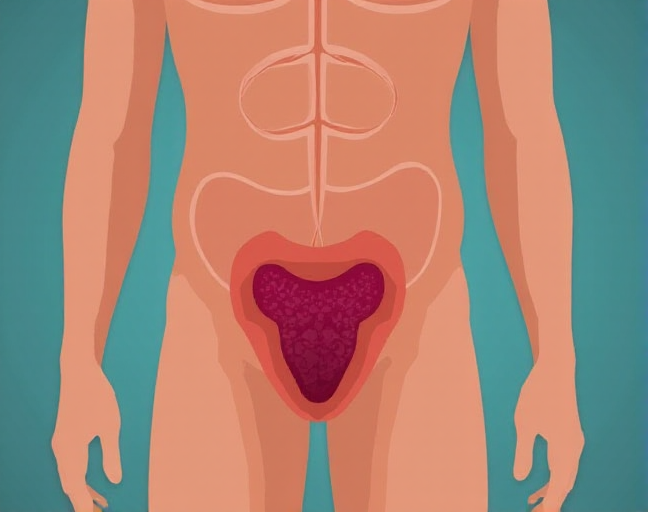
Testicular cancer is a type of cancer that begins in the testicles, where cells start growing uncontrollably and form a mass. While the exact cause isn’t fully understood, certain risk factors can increase the likelihood of developing this condition. Though it can be serious, testicular cancer is one of the most treatable cancers, especially when caught early. That’s why regular self-exams are so important. Let’s explore the possible causes of testicular cancer to help you stay informed.
What Causes Testicular Cancer?
Testicular cancer starts when healthy cells in the testicles turn cancerous. Normally, cells grow and divide in an orderly way, but when something goes wrong, they multiply out of control, forming a tumor. Most testicular cancers begin in the germ cells (the cells that produce sperm), but the reason behind the transformation remains unclear. However, several factors might contribute to this process.
1. Undescended Testicles
In babies, the testicles initially grow inside the abdomen and later move down into the scrotum. If this doesn’t happen, a condition known as undescended testicles occurs. Boys who experience this may need surgery to correct it. If surgery happens after the age of 13, however, the risk of developing testicular cancer is five times higher.
2. Previous Testicular Cancer
If you’ve had testicular cancer once, your chances of getting it again increase significantly. You’re 12 times more likely to develop cancer in the other testicle. Regular follow-ups with your doctor are essential after recovering from this disease to monitor your health.
3. Age and Race
Testicular cancer is most common among young and middle-aged men, particularly those between the ages of 15 and 49. It’s also more frequent in white men, especially those in Western and Northern Europe. So, if you’re in this demographic, it’s good to stay vigilant.
4. Family History
If a close relative, like a father or brother, has had testicular cancer, your chances of developing it rise by six times. Researchers believe that genetic factors might play a role in this, suggesting that inherited mutations may contribute to the risk.
5. Endocrine Disruptors
Certain chemicals, known as endocrine disruptors, have been linked to testicular cancer. These include substances like polychlorinated biphenyls (PCBs), dibutyl phthalate (found in cosmetics), and some pesticides. Even though many countries have restricted these chemicals, exposure can still occur through contaminated food.
6. Infertility
Infertility is another potential risk factor for testicular cancer. Studies show that infertile men are three times more likely to develop this cancer, so if you’re dealing with fertility issues, it’s important to stay aware of your health.
7. Smoking
If you smoke more than 20 cigarettes a day, your chances of developing testicular cancer double compared to non-smokers. So, putting out that cigarette may not just be good for your lungs—it could reduce your cancer risk too.
8. Height
Here’s an interesting one: Studies suggest that taller men may have a higher risk. Men over 6.1 feet tall are twice as likely to develop testicular cancer, and this risk triples for those over 6.4 feet tall. However, being shorter than 5.6 feet seems to reduce the risk by 20%.
Symptoms of Testicular Cancer
Now that you know the possible causes, it’s crucial to recognize the symptoms of testicular cancer early. The most common sign is a painless lump in one of your testicles, typically about the size of a pea (though it can be larger). While not all lumps mean cancer, it’s important to check with your doctor. Other symptoms include:
- A sharp or dull ache in the scrotum or testicles
- A feeling of heaviness in the scrotum
- Fatigue and a general feeling of being unwell
- Fluid buildup in the scrotum
If you notice any of these signs, don’t hesitate to consult a healthcare professional.
How Is Testicular Cancer Treated?
Understanding the symptoms and causes is only half the battle. Once diagnosed, the next step is treatment. Fortunately, testicular cancer is treatable with several options depending on the stage and spread of the disease.
1. Surgery
The most common treatment involves removing the affected testicle (orchiectomy). The surgery is typically done through a groin incision, and if necessary, nearby lymph nodes may also be removed. Regular follow-up visits and tests, like CT scans and blood work, will help monitor for recurrence.
2. Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It may be recommended after surgery to kill any remaining cancerous cells. The side effects can include skin irritation, fatigue, and redness in the treated area.
3. Chemotherapy
Chemotherapy uses powerful drugs to kill cancer cells throughout your body. It’s particularly helpful if cancer has spread beyond the testicle. However, it comes with side effects like nausea, hair loss, and increased susceptibility to infections. In some cases, chemotherapy may also lead to permanent infertility.
By staying informed about the causes, symptoms, and treatments of testicular cancer, you can take proactive steps toward your health. Regular check-ups and early detection can make a world of difference when it comes to overcoming this disease.